Editors note: This is the second in a two-part series outlining key steps to help your facility prepare for the return of elective surgeries. Part 1 covers case prioritization and scheduling. Part 2 will cover day-of-surgery through patient discharge.
Recently we published a “how to” blog to prepare a patient for elective surgery. Now we have arrived at the day of surgery; this blog will describe key patient management strategies to keep both your patients and providers COVID safe through the procedure and into the recovery period.
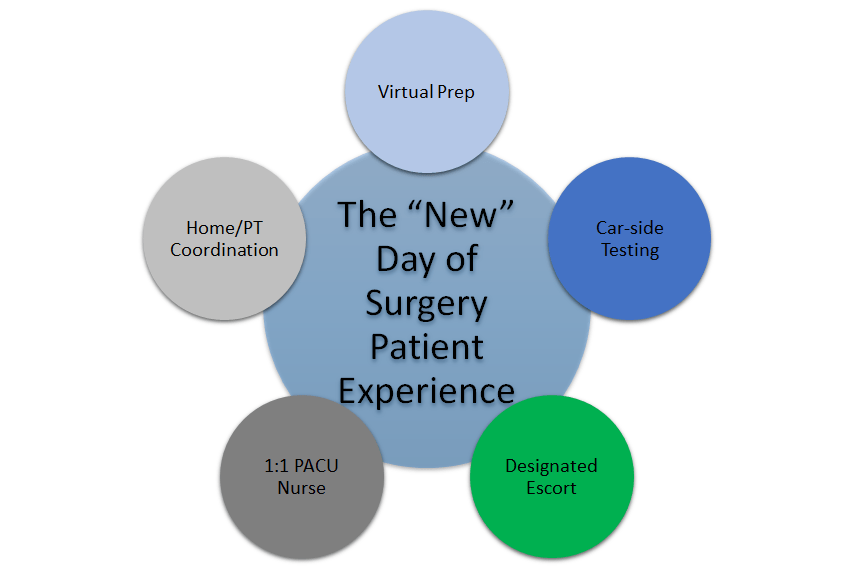
- Complete the education and registration process virtually. The primary objective here is for the patient to have as little nonessential direct contact with the hospital staff as possible. The patient preparation, expectations for arrival, discharge including the details described below, and post-op recovery education should be clearly communicated to the patient and their support person(s) either through a virtual pre-anesthesia visit or call. A second pre-op virtual health visit from the physical therapy department may be warranted.
- Upon arrival at the hospital, or ASC the day of surgery conduct car-side COVID testing. More testing is better. If your routine pre-anesthesia testing occurs more than three days before surgery, a second car-side COVID molecular test (using existing drive through COVID testing protocols) increases the probability a patient is COVID negative. This day of surgery test will re-assure the patient and your staff. Despite this rigorous testing, assume all patients are COVID positive. There is a false negative rate of up to 10% depending on the test.
- Designate escort personnel in PPE to take patient to the pre-op area and prep for surgery. Have the patient don an N-95 mask in the car. The patient should be escorted directly from the car staging area to the pre-anesthesia holding room. This concierge service will decrease the occurrence of patients roaming halls trying to locate the admission area and allows for proper queuing of patients into the pre-anesthesia holding room. It also prevents your staff from having multiple patient hand-offs before the patient arrives in pre-anesthesia holding. Patient’s family/support should be asked to wait in the car. While this is vastly different than pre-COVID scenarios, and may add to some patient’s stress, these protocols increase social distancing and decrease person to person interactions. Cell phone contact information for family/support should be acquired from those waiting outside the hospital to drive the patient home. If an overnight stay is expected, contact information and a post-op call from the surgeon replaces traditional post-op conversations in the family waiting room.
- Your Anesthesiologists will consider optimal anesthetic techniques to minimize PACU stay. Anesthesiology regional blocks have come a long way over the past 10-15 years. Now more than ever, it is important to utilize regional anesthesia in order to minimize dosing of pain medications and time in the PACU. An added benefit of blocks is improved patient satisfaction with less acute post-op pain.
- Designate a 1:1 single PACU nurse to manage the patient’s PACU stay and prep the patient for discharge. Again, the goal here is to minimize patient hand-offs among your staff. Depending on your facility, this PACU nurse may contact the driver by phone, give discharge instructions, and transport the patient to the car. Of course, scrupulous universal precautions and PPE use by the PACU team are essential. The patient should don an N-95 for the trip from the PACU to the car.
- Home health and physical therapy visits. Timing and services should be arranged at the time of booking. Ideally one identified nurse and/or therapist should be assigned to each patient with the understanding that those providers will be going to multiple patient’s houses. Decreasing the number of different providers visiting the patient’s home lessens the risk of cross contamination.
What about post op COVID testing? What if the patient was exposed after surgery and converted? Why test a patient 7 or 14 days post op? There are many opinions about post op COVID testing. In an ideal world where we have 100% reliable pre-op molecular testing, the post-op test could be avoided. Unfortunately, we do not have certainty. The goal of knowing if a post op patient is positive is to protect your staff and trace contacts back from a positive patient in order to decrease staff risk. We do not have enough data to argue for or against post-op testing. This illustrates the complex issues hospital and ASC leaders are navigating in real time.
So, how do hospitals and ASCs manage the mountain of opinion and data for safe return to elective procedures?
Surgical Directions can help.
Surgical Directions has spent 25 years in over 400 hospitals and healthcare systems improving efficiency, productivity, and quality. We are clinical professionals with decades of experience in patient care and health system leadership. We use advanced predictive analytics to mesh clinical results with business results. We understand your issues and are ready to assist with solutions. Please contact us for more information.



