A high-performing anesthesiology group is critical to the success of a hospital OR. Most OR leaders, however, do not know how to work effectively with anesthesia providers to define high performance and establish performance metrics.
Traditionally, anesthesia group contracts have not included detailed service standards. Language about anesthesia coverage is general, and the anesthesia provider’s role in ensuring efficiency and quality is not addressed. Crucially, most agreements do not offer a way to hold anesthesia providers accountable for meeting service standards. The most successful hospitals incorporate detailed OR and out-of-OR service standards into anesthesia group contracts. The key is to define expectations in four areas and establish effective performance metrics.
1. Coverage
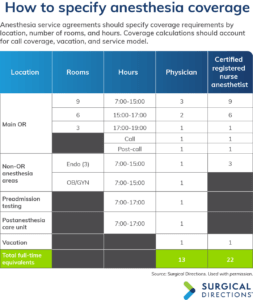
Most anesthesia group service agreements include coverage requirements, but the contract language is often vague. Many service agreements ignore key issues that are critical to defining coverage. When negotiating a service contract, work with your anesthesia providers to spell out coverage requirements in detail for both the OR and non-OR anesthesia areas (NORAs).
For the main OR, specify the number of rooms to be covered by day and by hour. Neglecting to define draw-down coverage can lead to chronic problems with late-day anesthesia provider scheduling. In addition, specify call coverage hours and availability expectations. Outside of call, define any weekend or holiday coverage needs and vacation staffing.
Well-constructed anesthesia group agreements define coverage requirements for all current and potential NORAs. Use historic procedural volume data to establish coverage needs for obstetrics, endoscopy, interventional radiology, the cath/EP lab, imaging, and any other anesthetizing locations. In addition, define staffing needs for anesthesia provider management duties in areas such as preadmission testing (PAT) and the postanesthesia care unit (PACU).
Service contracts almost always fail to address two important aspects of anesthesia coverage:
- Service model. Effective agreements specify whether the anesthesia department will use a physician-only or an MD/CRNA (certified registered nurse anesthetist) team model. The service model has a major impact on staffing and costs. Confusion on this point will create misaligned expectations between an OR, procedural areas, and anesthesia providers. The type of model directly affects the costs associated with any stipend or support required for anesthesia coverage.
- Add-on cases. Your service agreement should also specify that anesthesia provid- ers must accommodate add-on cases. The key is working with them to reach agreement on the definition of “urgent” and “emergent” cases through a governance committee.
It is also important to create mechanisms for accommodating changes in OR/procedural volume or service. Effective contracts require anesthesia leaders and hospital administration to review projected coverage and staffing requirements every 6 months. If case volume changes significantly, the OR/procedural director and the hospital chief executive officer should work with the anesthesia medical director and chief of anesthesia to negotiate appropriate changes in room commitments and staffing.
2. Clinical care
Most anesthesia service agreements take clinical care issues for granted. Viewing anesthesia as a commodity is a mistake because anesthesia service and quality can vary widely. Con- tract negotiations are an opportunity to set expectations for clinical care, competencies, and driving overall perioperative and procedural performance.
First, define basic anesthesia care parameters. The agreement should establish that anesthesia providers have responsibility for patients from preoperative evaluation through intraoperative anesthesia and postoperative care. The contract should specifically require anesthesia providers to:
- review all cases 3 to 5 days before the schedule
- personally see all patients with a status of American Society of Anesthesiologists (ASA) 3 or 4
- take part in daily clinical and operational huddles
- remain with each patient until their care can be transferred to PACU staff
- make sure all cases are appropriately documented in the medical record
- ensure that medication reconciliation is performed daily.
Effective service agreements also require anesthesia providers to take responsibility for perioperative processes and outcomes. Require them to develop algorithms and lab matrices for presurgical testing and establish evidence-based care pathways. All algorithms, tools, and protocols should be approved by the medical staff and the anesthesia department. Provider adherence ensures that all tests are both medically necessary and cost-effective, and that patients are optimized presurgically.
In addition, specify that the anesthesia group must:
- appoint a member to act as OR medical director
- manage and oversee the preoperative clinic/testing facility
- maintain a continuous quality improvement plan.
Anesthesia service agreements can also include program goals. For example, a hospital may look to the anesthesia department to develop a pain management pro- gram to improve outcomes and patient satisfaction or to lead a perioperative/surgi- cal home. These and other development goals should be included in the anesthesia service contract.
3. Leadership
Anesthesiologists are natural leaders in peri- operative services, and hospitals should give them a formal role in driving performance.
 Focus on four dimensions of OR leadership:
Focus on four dimensions of OR leadership:
Operations. Give anesthesia providers specific duties in day-to-day OR management. On a daily basis, they should assist the OR director and charge nurse with case scheduling. Anesthesia providers should also work with nursing to run the board, and the anesthesia medical director should address and resolve problems that arise with physicians.
Efficiency. Anesthesia providers should also take personal responsibility for daily OR efficiency. Contractual duties should include seeing all patients in the preoperative hold- ing area, making sure anesthesia consents are signed, and being present in the OR suite 15 to 20 minutes before incision. If a CRNA is not available, anesthesiologists should be ready and willing to start cases. Anesthesia providers should also assist with patient transport after surgery as needed.
Safety. Contracts should also leverage the anesthesia department’s ability to lead by example in patient safety. Require anesthesia providers to take part in time-outs. Anesthesia providers can also be commissioned to advocate for a just culture within the OR. Specific requirements could include developing a nonpunitive error reporting and review process.
Governance. If your hospital has a surgical services executive committee (SSEC), require the anesthesia department to appoint a member to serve as co-chair. Require the group to arrange the co-chair’s coverage commitments to ensure his or her avail- ability to fulfill SSEC duties.
4. Financial responsibility
If a hospital provides anesthesia with financial support, the anesthesia service con- tract must include standards to justify and validate the stipend.
Require the anesthesia group to meet a national benchmark for net collections, typically 97% or greater. As part of this requirement, the group must agree to submit to semiannual revenue cycle audits. Specify that if net collections fall below the agreed-upon threshold for two successive quarters, the hospital may reduce the stipend allowance.
Ensure accountability
Review anesthesia service on a quarterly basis, evaluating the group’s compliance with coverage requirements, care standards, and OR management responsibilities. Ideally, anesthesia provider performance review is conducted through a multidisciplinary SSEC.
Many elements of a service contract must be evaluated qualitatively, but it is possible to create hard metrics for measuring anesthesia provider performance (sidebar). For example, anesthesia-sensitive Surgical Care Improvement Project (SCIP) measures such as antibiotic prophylaxis, beta blockers, and perioperative temperature management are an effective gauge of clinical quality.
Service contracts can also require anesthesia providers to meet a threshold score on the Hospital Consumer Assessment of Healthcare Providers and Systems survey.
First case on-time start rates and cancellation rates are markers for efficiency, operational management, and leadership effectiveness. Performance thresholds can be upwardly adjusted over time, encouraging anesthesia providers to maintain performance gains and continuously improve.
As noted, net collections rate is the principal metric for tracking revenue cycle financial performance. Hospitals can strengthen accountability across all areas by reserving 25% to 35% of the stipend as an incentive payment. Tie the incentive portion to group performance on a range of key goals. For example, quarterly incentive payouts could be based on:
- SCIP compliance (30%)
- patient/surgeon satisfaction (25%)
- PAT leadership (25%)
- support for collaborative governance (20%).
- Overcome apprehension
Anesthesia providers are often apprehensive about service standards. Education and involvement will help overcome their concerns.
Collaborative governance gives anesthesia providers a strong voice in developing service standards. Centering the discussion in an SSEC makes the process more palatable for the anesthesia department. Service expectations come from a group of physician peers and nursing partners, not simply as a dictum handed down by hospital administration.
In poorly run surgery departments, schedule unpredictability makes it very difficult for anesthesia providers to ensure adequate and prompt coverage. OR leaders who expect anesthesia providers to accommodate add-on cases must create an efficient, vertical schedule with wise use of staff resources.
Don’t wait
In most hospitals, the service standard issue comes up only when there is wide- spread dissatisfaction with anesthesia performance. For hospitals that have not yet reached the “boiling point” with their anesthesia providers, contracting represents a valuable opportunity. These ORs should work with the anesthesia group to establish service standards and create effective performance metrics. A solid anesthesia service contract will help make strong gains in clinical and operational performance.
This column is written by the perioperative services experts at Surgical Directions (www.surgicaldirections.com) to offer advice on how to grow revenue, control costs, and increase department profitability.



