Problems such as frequently running out of critical items, expired inventory, and secret stockpiling in the OR have become increasingly burdensome for surgeons, nursing staff, and hospital administration across the country. Wasteful supply chain spending marginalizes patient care and drives OR expenses out of control.
“When the facility’s difficulties in maintaining sufficient inventory levels repeatedly interrupt and delay surgical schedules, all of those involved look for solutions that will bring immediate results,” says Barbara McClenathan, MBA-HCM, BSN, RN, CNOR, senior nurse executive at Surgical Directions, a Chicago-based healthcare consulting firm.
Tackling the typical challenges
The experienced clinical team at Surgical Directions has identified several common issues that crop up during their assessments of OR supply chain processes. “Many supply chain issues stem from untrained and undersupervised supply procurement staff,” McClenathan says.
When staff are tasked with ordering supplies without the benefit of usage-driven data or input from end users, oftentimes inventory quantities become skewed. This leads to complaints from surgeons about missing products, escalating costs per case, and overstocking of expired products.
Revamping supply chain management requires the collaboration of key stakeholders: surgeons, anesthesia providers, and executive and nurse leaders. These individuals should form a value analysis committee (VAC) to create guidelines for improving patient care and controlling product costs. The guidelines should be based on purchasing cost-effective, high-quality products and determining their clinical efficacy and financial impact.
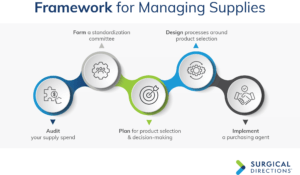
A five-step process is a good model to use for correcting course in how supplies are obtained and stocked, and how contracts are managed.
Audit
Conducting an audit involves tracking and benchmarking supply spend. The VAC should first develop a plan with metrics and goals that align with the mission of the facility. During this benchmarking phase, a complete supply audit of the OR should take place to identify wasteful spending trends.
Metrics can be categorized as macro and micro. Both should be tracked regularly and monitored for trends. Brian Watha, MHSA, LBB, director of process improvement at Surgical Directions, says typical ratios to monitor at a macro level include preference cards and supplies as a percentage of operating expense and as a percent- age of net revenue. A micro-level audit will demonstrate how often a nonpreferred vendor is used, for example, in total joints.
Tracking supply spend is essential, and it’s equally important to analyze the impact of those expenditures. Watha notes that hospitals often overlook metrics such as unused items on preference cards, shrinkage, obsolescence, and cost per case com-parisons by physician for the same procedure—all of which should be considered when trying to reduce costs.
Form a standardization committee
A standardization committee, which is a subset of the VAC, should be established to identify and maintain a minimal variety of comparable products. Many facilities stock the same product from multiple vendors, according to surgeon preference. Standardization or single sourcing of high-cost surgeon preference items—such as biologicals, mesh, vascular devices, orthopedic implants, and advanced energy and laparoscopic devices—offers significant opportunity to cut costs.
The greatest challenge of standardization is gaining surgeon consensus on prod- uct choice. Competing surgeons may be averse to trial products used by their peers. Brand choice and product performance are important to surgeons, in part because of the training they’ve received, notably for endomechanical and orthopedic devices.
Providing a comprehensive, hands-on trial with specific clinical evaluation indica- tors will help achieve consensus about product options. Choose a surgeon champion who is well respected by his or her colleagues, and have a consistent, well-defined decision-making process supported by senior leadership. In addition, have a policy for how to manage outlying requests. For example, surgeons who wish to use a non- standardized product should be required to provide written justification to support its clinical superiority.
Plan
Based on the results of the audit, the ad-hoc standardization committee can now serve as a multidisciplinary decision-making team that uses established processes to identify, grow, and sustain savings opportunities.
The VAC, composed of physicians, clinicians, and administration, provides input into product selection and decision making. The VAC unites surgeons and other clinicians with financial analysts and purchasing experts to make best-value product acquisition decisions.
Design
The VAC defines objectives related to the safety, performance, quality, clinical efficacy, and cost of products. The VAC should review and evaluate existing products as well as requests for new products.
A database to track cost savings related to new initiatives, ideally in a web-based platform, should be developed with a description of the initiative, products, estimated current annual spend, and estimated annual savings. A new product request form, including the guidelines, should be provided to perioperative service line leaders, OR buyers, and all stakeholders defined in the VAC charter.
Best practices are to:
- reduce expenses through product standardization
- purchase optimally priced equipment and devices
- use evolutionary provisioning, ie, require that existing shelf products be ex- changed or used before upgrading or converting to a different product.
Implement
Once the VAC has completed its evaluation and identified the supplies that are needed, a dedicated purchasing agent familiar with existing contracts and pricing agreements should negotiate the contract. The agent will analyze factors such as volume discounts, conversion credits, dependence on a single vendor, group purchasing discounts, or local contract discounts.
Contracts should be negotiated on the basis of standardization and cost-to-quality ratios as opposed to the traditional platform of best pricing. Bulk purchases that tie up capital resources or product conversions that lead to products sitting on shelves until expiration will consume more dollars than can be saved through price cuts.
Contract negotiation/renegotiation
The first step in contract negotiation is for the purchasing agent to identify and review existing contracts, vendor contracts that may conflict, or group purchasing organization initiatives. Local contracts exclusive of group purchasing negotiated contracts may not be desirable if they result in alternate tier-level reduction or if they are unable to meet volume rebates.
All pricing agreements must be aligned. For example, reprocessing of products such as tourniquets and sequential stockings could be easy, nonintrusive cost-saving initiatives. The downside is that the pneumatic tourniquet unit and sequential stock- ing unit may be provided to the facility free of charge based on disposable product usage. On the flip side, it may be more cost effective to purchase or lease the equipment rather than pay a higher price for each accompanying disposable item
Before a product conversion occurs, the purchasing agent should analyze existing inventory to define the value of overstock and expired products. The vendor must agree to provide credit or exchange the product. The second, less desirable strategy is to postpone product conversion until all shelf supplies are consumed. Many times, the OR buyer may not be in the loop for conversion, so product duplication may creep in
Finally, the purchasing agent should submit all applicable contracts to the VAC for periodic review. The committee will evaluate whether the conditions of the contract meet the current needs of the department and whether pricing is aligned with current market trends.
Sustain
Once a structure is in place for supply management, healthcare providers can shift their focus from inventory problems to optimizing patient care. Establishing this structure requires collaboration, meticulous data analysis, and a commitment to making changes that, if properly implemented and maintained, will strike a balance between providing the necessary supplies and achieving financial goals.
This column is written by the perioperative services experts at Surgical Directions (www.surgicaldirections.com) to offer advice on how to grow revenue, control costs, and increase department profitability.