Last Updated October 21, 2024
Turnover time is a major concern for OR leaders. We surveyed OR Manager readers last year to identify the business and efficiency issues they want to know more about. Reducing turnover times ranked second, just under cost control.
Extended turnovers clearly affect labor costs, but they also have a strong impact on surgeon satisfaction. And depending on the specialty, long turnovers can effectively shrink OR capacity and reduce profitability.
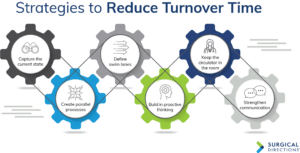
Reducing average turnover time is a complex challenge that calls for multidisciplinary collaboration. Many people contribute to the problem of inefficient turnover, so all OR stakeholders must work together to solve it. Six strategies are effective:
1. Capture the current state
The first step to improving turnover time is to observe your current turnover processes. Alecia Torrance, senior vice president of clinical operations at Surgical Directions, a consulting firm in Chicago, worked recently with an East Coast specialty hospital where the average turnover time was 40 minutes.
“Our first step was to get all the key stakeholders together in a room, including nurses, techs, anesthesia providers, and others,” Torrance says. “We asked them to describe the current turnover workflow. That helped us create a ‘current state map’ of the process. We then got special permission to videotape the turnover process.”
Three surgeons volunteered to have their turnovers recorded for an entire day. A videographer captured all activity from the time a gurney was wheeled out of the room until the arrival of the next patient.
Later, the group reconvened to review the video. “People were shocked when they saw how uncoordinated the turnovers actually were,” Torrance says. “It was remarkable but also kind of funny. Everyone laughed as they watched the same table get cleaned three different times during a single turnover.”
The value of the exercise was that it let everyone see that the process was broken. Staff then collaborated to define and map out a well-orchestrated turnover process. After months of work, the department succeeded in reducing average turnover time to 23 minutes.
2. Create parallel processes
One common problem is that many turnover tasks are performed sequentially. To reduce turnover time, staff should take advantage of opportunities to perform steps in a parallel fashion. Appropriately “stacking” processes helps shorten the entire turnover.
Here are a few examples:
Breakdown/cleanup. In many ORs, staff do not begin cleaning the room until the patient has exited. But from an infection control standpoint, many cleanup tasks can begin as soon as the dressing is on. For example, staff can remove trash, send unneeded instruments to sterile processing, and begin cleaning equipment.
Setup. Often OR staff do not begin preparing supplies until the patient is in the room. Supply setup can actually begin much earlier. Immediately after the room is clean, the circulating nurse can lay out supplies and begin opening sterile packs. Once the back table is set up, the surgical technologist can begin the preoperative count and the circulating nurse can complete his or her assessment of the next patient.
Anesthesia processes. Anesthesia teams can also perform more tasks in parallel. For example, 20 minutes before the end of one case, the anesthesiologist can place the line or administer a block for the next case.
3. Define swim lanes
Another problem in many ORs is that turnover responsibilities are poorly defined. Recall the “triple-washed” table mentioned above. Things like this happen because turnover task assignments are not clear. The results are redundancy, wasted effort, and extended turnover.
The solution is to establish “swim lanes” for all staff. A swim lane is a distinct set of tasks belonging to an individual team member. With well-defined swim lanes, the activities of nurses, surgical technologists, certified registered nurse anesthetists (CRNAs), and other staff can be streamlined.
For example, when the patient exits the operating suite, staff roles sometimes become hazy. Individual staff members may take up tasks according to convenience or preference. Cleanup proceeds slowly because no one is responsible for a dedicated series of tasks. In contrast, effective swim lanes for the minutes following patient exit could include:
- Surgical technologist—move instruments to the contamination area for reprocessing
- Float nurse—bag trash and linens
- Orderly/CRNA—mop floors and wipe lateral surfaces.
Defining responsibilities in detail allows staff members to perform tasks immediately and efficiently.
The swim lane concept does not mean turnover roles should be defined rigidly. In many cases, staff must be willing to take on tasks outside their traditional job descriptions.
“In some ORs, staff won’t begin the turnover until someone from environmental services takes out the trash,” says Yvette Stanley, project manager at Surgical Directions. “They were trained that removing trash wasn’t part of their job, and they may have been doing it that way for 15 years.”
Work with staff to examine turnover processes and look for teamwork opportunities. Changing attitudes about traditional roles can be difficult, but effective OR leaders can succeed by helping staff take pride in their efficiency and trust that the tasks are being performed per the prescribed methodology.
4. Build in proactive thinking
Many turnover plans do not take advantage of opportunities to “stay ahead of the curve.” Train staff to anticipate the process, not just react to problems and needs.
For example, staff members can initiate many turnover steps a full hour before the end of a procedure. When a procedure is approximately halfway completed, the circulating nurse can notify the charge nurse that a bed will be needed and also call for the next patient. The orderly or CRNA can check the case cart and identify any additional equipment needed for the next procedure. The anesthesia technologist can also begin readying supplies for the next case.
Many turnovers are extended simply because a gurney is not present when the patient is ready to exit the room. A little bit of proactive thinking resolves the problem. Train orderlies to retrieve a gurney 5 minutes before case completion.
5. Keep the circulator in the room
In most ORs, the circulating nurse is responsible for transporting patients from the preoperative holding area to the surgical suite. This allows the circulator to build rapport with the patient and assuage any patient concerns en route to the OR, but it also pulls the circulating nurse away from the OR during cleanup and setup, often leaving the scrub technologist to turn over the room. The circulator is absent precisely when he or she is most needed to manage an efficient turnover.
A better approach is to have the anesthesia provider and an orderly transport patients from the preoperative holding area to the OR. This allows the circulating nurse to stay in the room and facilitate turnover.
The anesthesiologist or CRNA is usually the last person to evaluate the patient in the preoperative holding area, making this an efficient solution. In addition, the anesthesia provider can answer any questions the patient may have during transport.
Similar inefficiencies occur during transport of patients from the OR to the post-anesthesia care unit (PACU). In many hospitals, the circulating nurse accompanies patients to the PACU, which means time is spent walking back m and forth instead of leading the room turnover.
One alternative is to have the anesthesia m provider transport the patient to the PACU, deliver the report, and then proceed directly to the holding area to complete the assessment of the next patient.
A second alternative is to have a PACU nurse come to the OR to retrieve patients. In most hospitals, PACU nurses have ample downtime. When available, a nurse can come from the PACU, receive the report from the circulating nurse, and then transport the patient back to the PACU along with the anesthesia provider.
A third alternative is to create a multi-utility role that combines functions to optimize productivity and efficiency. For example, transport, housekeeping, and operating room technician functions might be combined into one position.
6. Strengthen communication
“Communication is a huge aspect of efficient turnover,” says Barbara McClenathan, senior nurse executive at Surgical Directions. “Turnover processes cannot be well orchestrated unless all team members have real-time information.”
Key points include:
Instruments. “Say a vendor representative brings in two instrument trays for a surgeon who has scheduled three total hip replacements,” McClenathan says. “The tray used during the first case must be processed in time to allow the third case to begin promptly.” OR staff need to stay in close contact with sterile processing staff in order to manage this tight turnaround.
Equipment. Delays in locating and moving C-arm systems, laparoscopic video towers, surgical microscopes, and other equipment can lead to extended turnovers. Staff must inform other team members when a room is clean so any needed equipment can be brought in promptly.
Patient readiness. Turnovers run long when there are delays in preoperative medical orders or laboratory tests. In-room staff must communicate with the pre-operative holding area to make sure patients will be ready when their room is ready.
For example, when a surgeon begins to close an ophthalmology case, OR staff should send an update to the preoperative holding area team so that they can then administer eye anesthetic and dilating agents to the next patient.
It is important to use an effective communication system. “Many ORs still use telephones to communicate, but this can be inefficient,” McClenathan says. “You may need to make five or six different calls just to coordinate the next patient.” Tracker boards offer efficiencies, but many ORs are not using them to their full potential. “Sometimes boards are installed in only one or two locations,” she notes.
Some ORs have begun using communication systems accessible by smartphone or tablet. McClenathan believes voice solutions are still effective: “Some of the newer software-driven solutions integrate voice, smartphone, and tracker capabilities.”
Measuring and monitoring turnover
The keys to any improvement effort are to measure the objective and to monitor performance consistently.
When working to improve turnover times, begin by establishing the current performance baseline. The primary turnover efficiency metric is “wheels out to wheels in” time. An additional metric for measuring turnover performance is “close to cut” time.
Once you have established baseline measures, monitor ongoing performance and post data where it can be seen by physicians and staff.
The Hawthorne effect—also known as the “observer effect”—will yield a net benefit over and above any process improvements. When team members know their performance is being observed through data monitoring, they will execute turnovers more efficiently.
Multiple benefits
Reducing turnover times can significantly improve surgeon and patient satisfaction. Improving time efficiency can also increase department capacity so that more cases can be accommodated without increasing indirect costs.
This column is written by the perioperative services experts at Surgical Directions (www.surgicaldirections.com) to offer advice on how to grow revenue, control costs, and increase department profitability.