Is your preanesthesia testing area providing measurable value, and is it positioned to drive surgery toward a new paradigm of care? As government payers shift toward value-based care with the required bundled payment for total joints starting in 800 hospitals and 75 markets (as part of the Comprehensive Care for Joint Replacement Model), OR directors should be asking, “How is my preanesthesia testing area positioned to help embrace and lead this change?”
During the budget cycle, senior administrators often question the value of the preanesthesia testing area (PAT) because it is not a revenue-generating area of the hospital. Each full-time employee is then scrutinized for value and productivity. However, in most hospitals where providers have been fragmented into employed, aligned, and splitter surgeons, the lack of an effective PAT means patients often arrive at the hospital without lab test results or diagnostic studies. Thus, charts are incomplete, and getting patients ready on the day of surgery becomes a fire drill.
In this article, perioperative services experts at Surgical Directions, a Chicago-based healthcare consulting firm, will explain the role of PAT in ensuring that patients can safely undergo planned surgical procedures and that the facility can meet regulatory requirements for documentation.
ROI for PAT
In an effort to curb costs, surgeons’ offices are increasingly using less expensive, poorly trained workers. Extracting good clinical information is a challenge, yet in budget meetings, the rallying cry is, “Aren’t we paying for a service the surgeons should be doing anyway?”
It may be tempting to reply, “If the hospital staff were expected to enter all the historical health information, medications, and allergies on the morning of surgery, no surgical case would ever start on time,” but there is a more definitive approach to answering administration’s concerns.
The answers are not simple, but a return on investment for PAT can be calculated. The Centers for Medicare & Medicaid Services (CMS) has shifted the focus to value, which means PAT must move from a data-gathering resource to a perioperative and risk reduction center. Such is the case with top-tier organizations as they look toward a full comprehensive care bundle.
Surgical directors and managers may use a variety of metrics that drive staffing for the OR. Most often, productivity is measured using surgical minutes or cases. This becomes a challenge for PAT because the nurses and staff hours may be accurately correlated to this metric, but in some instances, PAT may provide no direct patient care. Measuring performance is complex because some centers do only calls, others do only visits, and many do a mix of both. PAT nurses may be spending much of their time working with the electronic health record (EHR) and on the telephone.
Value vs cost
In our new paradigm, we define value as quality divided by cost. With regard to PAT, how are value and cost per patient measured? One way is to measure the cost of service per patient evaluated. Cost per patient may be calculated by totaling the clinical and clerical staff expense +/- overhead expenses ÷ the total number of patients evaluated (by phone or visit). Another way is to subtract the revenue from laboratory testing done at the center. The costs vary widely at different sites, but we use a benchmark of <$50 per patient.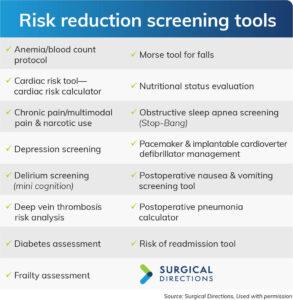
On the quality side, one need look no further than cancellations or delays caused by medical reasons as a justification for PAT. A 2012 study at Tulane University in New Orleans reported that, for 10 different surgical specialties, the average cost of cancellation was $2,924. Using this benchmark and tracking cancellations by reason, one can apply the following formula:
Total cost = total cancellations for medical reasons x total number of cancellations.
Costs of delays caused by inadequate clinical information, optimization notes, or a blank nursing database on the morning of surgery are quantifiable by multiplying total minutes delayed by a published benchmark cost per OR minute of $30. Surgical Directions has long used a benchmark of <1% cancellations with a 95% on-time start. If PAT is not providing the value an organization demands, a thorough analysis is warranted to uncover deficiencies and create a targeted action plan.
Resource needs
Part of any quality evaluation is a clear map of the current processes and tools available to the PAT staff, with a careful review of the EHR. Are all providers documenting in one record, or is the EHR a hospital-based record that requires redundant documentation of all clinical information from outside providers? Often not all providers are on the system, and getting clinical information from them costs time and money.
Observation and timing of staff placing calls and conducting visits are also very important in determining how staff are allocated. We strongly recommend allowing 50 minutes for visit times and 40 minutes for call appointments. Both calls and visits should be scheduled.
Setting expectations for time and determining how many calls or visits a provider accomplishes during a shift is a way to distinguish high and low performers. Using the high performer as an example can help to bring all staff into alignment.
Every workstation should have dual computer screens, and providers should review available clinical information prior to initiating a call or visit. Knowing the health history of the patient before arrival cannot only help the patient feel that the team is prepared but also allows more time for education and questions.
In conducting a Lean Six Sigma evaluation of current processes, it is essential to review which tools staff are using. Anesthesia providers’ involvement in the pre-surgical evaluation process is critical, and they must approve the tools used in PAT.
Three required tools include:
- laboratory matrix by procedure and comorbid disease
- medication management matrix
- abnormal lab test guidelines.
Laboratory guidelines
PAT testing has come under intense scrutiny because much of the testing has uncertain value, as demonstrated by the exhaustive review published by the Agency for Healthcare Research and Quality. Their study cited the clear lack of value for pre-surgical testing for cataract extraction in impacting outcomes. Additionally, electrocardiograms (ECGs) received a “D” score for usefulness by the US Preventive Task Force in its 2012 study.
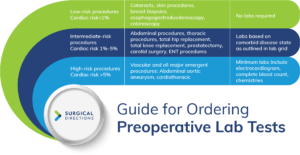
Reducing preoperative laboratory testing is a big focus for many top-tier systems as they prepare for bundled payment and capitated care. Currently, CMS will not reimburse providers for hospital-based lab studies that are not completed within 72 hours of hospital admission. In the future, bundled payment timing will likely be irrelevant, but for now, careful attention should be paid to ensure full reimbursement for every case. A grid approach can be used to determine the need for lab studies. This grid should drive decisions based on both
the complexity of the surgery and the patient’s comorbid disease state. Many organizations have adopted a guideline for accepted results of ECGs for 6 months to 1 year and chemical lab tests for at least 3 months, provided there has been no change in the patient’s health. The anesthesia department’s grid for specific lab tests based on a patient’s comorbid disease state should be used in conjunction with this guideline.
Decision makers must review a patient’s lab test results before the day of surgery. Not every abnormal lab test based on a lab test’s parameters needs follow up. Many PAT staff hours are spent chasing abnormal results that will never cause a case cancellation. The anesthesia group should develop an accompanying abnormal lab test grid with result values that may put a case at risk for cancellation.
Medication management
All providers should work from a standardized document for managing medications prior to surgery. Seeking input from pharmacy, medical specialists, and published evidence will help guide a clear protocol for medication management. Particular attention must be given to antidiabetics, antihypertensives, diuretics, and anticoagulants.
With all of the new anticoagulants on the market and increasing use of regional blocks and catheters, it is essential to have a strategy for managing anticoagulant medications. All PAT providers should identify patients who have had a cardiac stent or need bridging therapy for mechanical heart valves and those at high risk for deep vein thrombosis. Before changing any anticoagulant, consult with the patient’s cardiologist or the prescribing provider.
Regardless of whether calls only, visits only, or a mixed process is used,
staff deployment is key to optimal productivity. Decide how many staff are needed to serve the patient population, and then deploy one to three of the staff nurses as the abnormal or “abby nurses” who contact providers when additional clinical information is needed. As the date of surgery approaches, the “abby nurse” understands the full clinical history of the surgical patient. Any patients with special needs should be reviewed in the daily OR huddle.
Risk reduction strategies
In addition to the routine evaluation of a patient’s past clinical history, many PATs are beginning to evaluate a wide variety of conditions and issues that may impact post surgical outcomes. Factors that may affect a patient’s “wellness” for elective surgery should be considered. Leading PATs are leveraging these screening tools and developing supplementary care management processes. Some PATs are renaming their clinics as perioperative risk reduction clinics.
A paradigm shift is underway in healthcare that ties reimbursement to the value proposition quality divided by cost. The PAT department can lead in this endeavor and can be the catalyst for developing a perioperative surgical home. In addition, PAT is the place to draw up a discharge plan with input from hospitalists, anesthesiologists, risk reduction nurses, nutritionists, case managers, and other professionals responsible for providing a comprehensive plan of care for all surgical patients.
References
Agency for Healthcare Research and Quality. Benefits and harms of routine preoperative testing: Comparative effectiveness. Executive Summary. January 29, 2014. http://effectivehealthcare.ahrq.gov/index.cfm/search-for-guides-reviews-and-reports/?pageaction=disp layproduct&productid=1847
http://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/coronary-heart-disease-screening-with-electrocardiography
Macario A. What does one minute of operating room time cost? J Clin Anesth. 2010;22(4), 233-236.
McCook A. Cancelled surgeries costing hospitals millions. Anesthesiology News. 2012;38(5), 1, 23.



