Last Updated October 21, 2024
Surgical Services is the Key to Financial Recovery
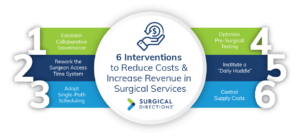
Maximizing perioperative services in the post-COVID era is essential to financially recovering from the pandemic. In a recent survey led by Surgical Directions, more than 95% of hospital executives indicated that optimizing surgical services was critical to their COVID-recovery strategies. However, less than 50% believed they were well positioned to actually accomplish that objective. Surgical services at most institutions represents more than 60% of total revenue, yet accounts for a disproportionately higher level of contribution margin. The key to financially stabilizing organizations today lies in increasing productivity out of the operation room. This white paper from Surgical Directions describes six interventions that will transform your OR into a high-margin driver of hospital financial performance.
 1. Establish Collaborative Governance
1. Establish Collaborative Governance
A shared governance model will set the stage for efficiency gains and volume growth.
Problem:
Most hospital ORs are governed by a committee of the medical staff. This committee typically focuses on medical staff dynamics, not organizational performance. The OR nursing director has authority over operations from a nursing perspective but is not empowered to lead effective change. No leadership body is accountable for the overall performance and strategic success of surgical services. As a result, the OR is a static organization, operating in functional silos, that lacks the impetus to improve. Ultimately, the OR fails to serve its core customer: surgeons.
Intervention:
Create a governance structure that engages all the stakeholders with a vested interest in OR operations—surgeons, anesthesia, nursing and hospital administration.
Leading hospitals have established strong multi-disciplinary leadership by creating a Surgical Services Executive Committee (SSEC). An SSEC is a multidisciplinary “board of directors” for the OR. Members include clinically respected surgeons and anesthesiologists, nursing leaders, hospital senior executives and ad hoc representatives from key ancillary departments. Importantly, the SSEC is sponsored by hospital administration and typically reports to the hospital president and CEO. Because the SSEC is a committee of the hospital (not the medical staff), it is able to focus on the overall performance of the OR. Since the committee includes clinicians, department managers and hospital leaders, it is able to address problems from every angle. It provides a forum to address surgeons’ needs and empowers anesthesia to spearhead operational improvements.
The SSEC’s job is to create a strategic vision for the OR, develop a formal growth strategy, sponsor process improvement and guide cultural change. The SSEC also functions as an operational committee for the surgery department. Members meet frequently to review OR data and address performance problems.
Outcomes:
Establishing a multidisciplinary SSEC will set the stage for key improvements in OR operations, financial performance and strategy.
- The SSEC provides a collaborative forum for implementing complex operational improvements, such as improvements in block time allocation, and as a peer-driven entity, create clear guidelines and transparent processes to manage potentially politically charged issues.
- The SSEC provides oversight of task forces assigned to critical elements within the perioperative service continuum, such as scheduling, presurgical testing and OR staffing. These collaborative initiatives are critical to reducing waste and inefficiency.
- Ultimately, the SSEC is key to creating a surgeon-focused environment that supports successful market strategy and volume growth.
2. Rework the Block Time System
A properly designed block schedule system increases OR utilization and case revenue.
Problem:
Most hospital ORs have an inefficient block schedule system. Block lengths are not optimized to make the best use of OR time. In addition, block rules are not aligned with the OR’s operational and financial priorities. The result is low utilization, which represents wasted capacity, wasted resources and under-performing department revenue. Block time inefficiency also creates access problems for surgeons, particularly less-tenured physicians. Overall, block time problems lead to moderate-to-severe problems in costs, profitability and organizational effectiveness.
Intervention:
Task the SSEC with developing a new block time system that optimizes OR utilization and ensures access for the most active surgeons. Effective block time systems share five common characteristics:
- Minimum block length: Assign block time in increments of 8 to 12 hours. Unlike traditional 4-hour blocks, longer blocks enable higher utilization per hour and minimize inefficiencies caused by frequent specialty changeover. There are exceptions to this guideline, based upon identified variables.
- Utilization threshold: Require surgeons to achieve at least 75% utilization to maintain their assigned block. If a surgeon cannot maintain adequate utilization, subtract entire blocks from their schedule—do not shorten existing blocks. A higher threshold may be presented for an employed/captive model.
- Individual block ownership: Assign blocks to individual surgeons, not specialties or groups. Personal blocks create a sense of ownership that encourages optimal utilization. Academic institutions may create specialty-specific blocks, provided the institution possesses strong leadership from Chairs/Chiefs of Specialty/Surgery.
- Voluntary and Specialty-specific block release: Create a block time release matrix that enables the OR to fill unscheduled time. Specialties that treat many emergent cases may retain block time until 24 hours before the schedule. Blocks for elective-heavy specialties should auto-release several days ahead. Create a block time voluntary release protocol that enables the OR to fill vacated time due to vacations, CE/ CME, sabbaticals, etc. Typical voluntary release is thirty business days without penalty for block utilization calculations.
- Room flexibility: Create flexibility in the schedule by reserving approximately 20% of rooms for open time, urgent and emergent cases.
Outcomes:
An effective block time system will enable the OR to use time resources much more efficiently. Under many scenarios, a well-managed 8-hour block will typically accommodate 5.2 hours of operative time equating to four or five surgical cases, as compared to successive 4-hour blocks that may accommodate as few as three cases total. Better utilization will increase OR revenue and improve the department’s cost structure. Surgeon satisfaction will increase due to greater productivity. Transparent rules and peer administration establish a sense of fairness in the system. In addition, higher utilization enables anesthesia to attend more cases per day, increasing anesthesia income and satisfaction. Structuring blocks creates a more predictable schedule, improving nursing satisfaction.
3. Adopt Single-Path Scheduling
Optimal scheduling processes help reduce costs related to inefficiency.
Problem:
Many hospitals do a poor job of capturing and coordinating patient information prior to surgery. OR schedule requests are received through a variety of routes—phone calls, faxes, e-mails, written notes and verbal requests. Typically, requests lack full detail on the patient and the procedure. Lack of information creates many opportunities for inefficiency and waste. It also increases the risk of quality problems and adverse patient outcomes.
Intervention:
Create a standardized single-path scheduling system designed to ensure the capture of complete patient and procedure information.
The foundation of an effective scheduling system is a single, standardized process to schedule a case. Typically, a standardized schedule request fax form is the answer. A multidisciplinary task force should design the form to capture all the information required to prepare for a case and to identify high-risk patients. Mandatory fields should include: complete procedure description information, CPT code, anesthesia requirements, patient co-morbidities, patient allergies, testing and preventive care orders, and special equipment needs.
To effectively manage documents within the process, consider adopting a software solution that digitizes, indexes and stores all incoming faxes. Assign nursing staff to review all items upon receipt and sort them into electronic patient folders. The software and associated processes will coordinate scheduling forms, lab reports, imaging reports, consults and other patient documentation. The system ensures that all critical documentation is available as needed and that the patient is fully optimized prior to the day of surgery.
A key part of creating a single-path scheduling system is to develop a “new state map” of the targeted scheduling process. The map should trace the flow of information from the point a case is entered into the system, through staff tasks and responsibilities. Case management and discharge planning should also be a parallel component of the scheduling process.
Outcomes:
A well-designed single-path scheduling process will reliably capture all the information needed to ensure a safe and efficient surgery.
- Capturing information early—and ensuring a prompt clinical review—prevents many last-minute problems that can lead to case delays and cancellations.
- Reducing delays and cancellations optimizes OR utilization, costs and revenue.
4. Optimize Pre-Surgical Testing
A well designed pre-surgical testing clinic reduces case delays and late cancellations.
Problem:
In many hospital surgery departments, presurgical preparation is haphazard. Clinical staff do not follow standard protocols for preoperative testing, and preoperative management is poorly coordinated. As a result, many patients arrive on the day of surgery with incomplete tests, incomplete paperwork and unmanaged medical conditions. Ironically, a significant percentage of patients receive excessive testing, leading to high costs. In addition, testing that takes place for elective procedures within 72 hours of surgery are considered bundled in the DRG payment and cannot be compensated separately under CMS payment policy. Patients not optimized prior to surgery have increased risk for greater length of stay, subpar clinical outcomes and underwhelming patient satisfaction.
Intervention:
Develop a standardized pre-surgical testing process that ensures all elective surgical patients are evaluated a minimum of 3 to 5 business days prior to surgery.
The core of an effective process is a set of standard protocols and algorithms—developed under the leadership of anesthesia and hospitalists—for pre-surgical testing and patient management:
- Phone triage: Step one is to develop a risk assessment questionnaire that clinical staff can use to triage patients within 24 hours of being scheduled. Higher-risk patients should be directed to the hospital for an on-site assessment.
- Testing matrix: Anesthesia should also develop standard protocols for preoperative testing based on surgical invasiveness and patient co-morbid conditions.
- Lab result guidelines: Clinical staff need guidelines for assessing lab results in a consistent manner and managing abnormal labs.
- Prep protocols: OR leaders should also develop protocols for the preoperative management of patient co-morbidities, such as diabetes, hypertension and COPD. Anesthesia should perform a preoperative chart review for all high-risk patients with collaboration with hospitalists. Hospitalists can bill for a level III, when appropriate. Hospitalists can assist with pre-and post- surgical patient care to optimize clinical outcomes. In addition, create an on-site pre-surgical testing clinic for coordinating patient information and conducting on-site evaluations of higher-risk patients. Starting at time of surgical scheduling and after a MRN has been established, clinic staff should actively manage cases to ensure complete patient preparation.
Outcomes:
An effective pre-op process will help OR staff identify and manage patient health issues well ahead of time, ensuring that patients are completely prepared for their surgery. Full patient preparation reduces delays and cancellations. It also has the potential to reduce complications that require additional care and can lead to hospital readmissions and reduce length of stay. In addition, performing the bulk of elective case pre-surgical testing more than 72 hours prior to surgery allows the hospital to recoup testing costs through appropriate billing.
5. Institute a “Daily Huddle”
Cross-disciplinary communication improves schedule flow and optimizes resources.
Problem:
The processes that lead up to a surgical procedure come together rapidly on the day of surgery. Safe surgery requires fully orchestrated patient information, patient preoperative management, clinical staff, surgical supplies and OR facilities. Problems and issues discovered late in the process can easily lead to a delayed or cancelled case. In addition, last-minute decision-making can lead to waste—the procedure gets done, but not with the most efficient use of resources.
Intervention:
Establish a “Daily Huddle” process to systematically ensure that all the elements of a safe, efficient surgery are in place the day before a procedure.
- The “Daily Huddle” is a brief meeting held every day in the early afternoon for the purpose of coordinating the OR schedule.
- The meeting includes representatives from nursing, anesthesia, PAT, scheduling, materials management and other support areas.
- During the ”Daily Huddle,” participants review current-day problems and schedule issues, then preview cases scheduled for the following day and two–four days forward.
- Clinical staff in the huddle verify that patient charts are complete, all tests have been performed and all health issues have been appropriately managed.
- The “Daily Huddle” participants also check the schedule for any anticipated practical problems. Are allotted case times appropriate? Are any special supply requirements in place? Are there any resource conflicts? Are there anticipated delays in day of testing requirements to move the case later in the day? Problematic cases are resolved or rescheduled.
Outcomes:
Examining issues from a clinical perspective a day ahead of time enables the OR to prevent many problems on the day of surgery. This reduces cancellations and delays and helps the OR maximize utilization. The “Daily Huddle” process can also help the OR avoid potential quality problems that lead to complications, errors, increased length of stay and readmissions.
6. Control Supply Costs
A suite of effective supply chain management strategies helps reduce variable costs.
Problem:
Non-labor costs or surgical supplies represent a large portion of OR expenses, approximately 60%. Supply and materials costs are a particular problem with many high-revenue procedures. High costs associated with orthopedic, neuro and cardiovascular surgeries suppress the profitability of these specialties. In some cases, hospitals actually lose money on cases that should be major revenue drivers.
Intervention:
Implement supply chain management strategies that address the problem of high costs from multiple angles. Successful ORs use a range of techniques, such as:
- Educate surgeons: Develop cost-per-case dashboard reports and share them with surgeons. When surgeons see how their costs compare with reimbursement and to their peers, most will take a hard look at their supply choices. Involving surgeons on the value analysis committee will further engage them in cost control efforts.
- Educate OR staff: Nurses and other clinical staff should also be exposed to cost dashboards. In addition, educating staff about the cost of common supplies will help focus nurses on reducing waste. Conduct waste audits to identify supply categories that present the greatest savings opportunity.
- Individual block ownership: Assign blocks to individual surgeons, not specialties or groups. Personal blocks create a sense of ownership that encourages optimal utilization. Academic institutions may create specialty-specific blocks, provided the institution possesses strong leadership from Chairs/Chiefs of Specialty/Surgery.
- Reduce inventories: Work with staff to set rational par levels and reorder quantities for supplies (because there is a tendency to order excessive emergency stocks). Make a focused effort to spend down inventories, especially for high-cost items on a FIFO methodology. Renegotiate vendor agreements so that high-cost implants are held on consignment, not owned. Attempt to develop a perpetual inventory system or mimic just-in-time inventory management to improve annual inventory turns. Better performing institutions produce 12-14 annual OR inventory turns.
- Cap vendor prices: Set price caps on common high-cost procedures, such as joint replacements. First, assign target supply costs (you can use medical staff data to identify surgeons with consistently low costs per case). Second, communicate to surgeons and vendors that unapproved products will not be reimbursed.
- Plan for ROI: Perform a complete cost/benefit analysis (CBA) for all high-cost equipment purchases. Consider projected case volumes and projected revenue. A good CBA process will help the OR avoid wasting money on bad equipment investments—and ensure that good investments pay off through proper capital budgeting and management. The process should be incorporated into the value analysis committee scope.
Outcomes:
Physician and staff education, improved inventory management and better management of vendor relationships can lead to significant cost control gains. Many ORs are able to reduce non-labor expenses and control spending on high-cost implants and technology. Perpetual inventory systems create the opportunity to provide a one-time reclassification of inventory from the income statement to the balance sheet. Obsolescence and expired items will be reduced dramatically.



