Hospitals Depend on The OR to Drive Performance

Strong OR performance is critical to creating a sustainable hospital business model. In better-performing hospitals, the OR accounts for over two-thirds of gross revenue, drives up to 60% of the operating margin and creates strong engagement with the physician community.
Unfortunately, most hospital ORs struggle with a range of efficiency, cost and physician satisfaction problems. These problems create a “negative performance cascade” that ends in poor financial outcomes.
- Poor OR performance has always been a problem for hospitals.
- Today, declining payment, healthcare reform and difficult market trends are placing new pressure on hospital ORs.
- Poor performance in the OR is no longer acceptable.
- Hospital executives must work with OR leaders to make critical organizational and operational changes.
- Transforming the OR is the key to achieving strong strategic and financial performance for the hospital as a whole.
Case Study: Memorial Regional Hospital
Memorial Regional Hospital is a 553-bed acute care medical center in Hollywood, Florida. The hospital is situated in the southern half of the competitive Fort Lauderdale market, and it is located just 20 miles north of Miami.
Memorial Regional is the flagship facility of the third-largest public health system in the U.S. It has a long tradition of providing quality surgical care. In recent years, however, the surgery department slipped into a pattern of underperformance.
Situation: Low Efficiency Driving Poor Financial Outcomes
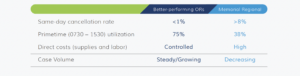
Disorganization in the OR was leading to a range of problems, including an extremely high cancellation rate. Cancellations and other problems created chronic delays in the OR schedule. In addition, OR utilization was very low, creating a high cost structure that ate into profitability.
- Surgeons were dissatisfied with the inefficient working environment. During the same number of hours, surgeons were able to perform about 30% fewer cases at Memorial Regional than other hospitals.
- The anesthesia department was also frustrated. Low utilization translated directly into low productivity and charges, leading to low income for anesthesiologists.
- High OR costs and declining case volumes reduced hospital operating margins.
Intervention: Establish Physician-Led Governance for the OR
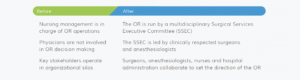
Executive and surgery department leaders at Memorial Regional came together in 2012 to make strategic changes. Their first step was to create an effective governance structure for the OR.
Memorial Regional established a Surgical Services Executive Committee (SSEC) in November 2012. The committee functions as an operational “board of directors” for the OR.
- The SSEC is co-chaired by a surgeon and an anesthesiologist, and it includes active surgeons from a range of specialties.
- Hospital executives hold seats on the SSEC, but they forego voting rights to show their support for physician leadership.
- The goal of the SSEC is to allow surgeons and anesthesiologists to take personal responsibility for the OR.
Intervention: Create an Effective Block Time System
The SSEC’s first priority was to reform Memorial Regional’s ineffective block schedule system. Committee leaders worked with the medical staff to design and implement new rules and expectations.
Block length: The existing system included a mix of longer blocks and short 4-hour block
Issue: Short blocks cannot be utilized efficiently, leading to excessive downtime
Solution: The SSEC now allocates OR time in 8-hour and 10-hour units exclusively
Ownership: Many blocks were assigned to specialty services or surgeon group practices
Issue: Group ownership diminishes individual responsibility
Solution: Blocks now are assigned primarily to individual surgeons, creating a sense of responsibility for full utilization
Utilization standards: Block time utilization requirements were not enforced
Issue: Unenforced standards contribute to the problem of low OR utilization
Solution: The SSEC mandated that surgeons must maintain a utilization rate of 75% in order to maintain block ownership
Release: Previously, unscheduled block time was released only shortly ahead of the day of surgery
Issue: A short release system does not give OR management the opportunity to fill unscheduled time
Solution: The SSEC established a specialty-specific release schedule that facilitates better schedule management
Access: Under the existing system, very little OR time was open to non-blocked surgeons
Issue: Lack of open access makes it hard for surgeons to schedule add-on cases; and newer surgeons cannot access the schedule
Solution: The SSEC designated about 20% of capacity as “open rooms” to accommodate add-ons, urgent/emergent cases and non-blocked surgeons
Intervention: Reformed Block System Launched
The SSEC introduced the new block time system to surgeons in spring 2012.
- All surgeons were required to reapply for block time
- The SSEC reallocated block time based on surgeons’ historic utilization data
- The new system was formally launched in May 2013 The SSEC began monitoring surgeon utilization rates
- Block time is periodically reallocated to reward the most efficient physicians
Intervention: Build Quality and Efficiency into Pre-Operative Processes
A large percentage of cases were cancelled on the day of surgery because patients were not fully cleared for their procedure. Common issues included incomplete labs and lack of medical clearance. The SSEC addressed this problem by strengthening pre-surgical processes, ensuring that patients are fully prepared and medically optimized on the day of their surgery.
- Info capture: New upfront processes capture complete information about the patient and the procedure.
- Scheduling: Staff now schedule cases by CPT code to ensure accurate procedure details, appropriate patient preparation and optimal supply management.
- Standardized testing: Anesthesiology leaders developed standard pre-surgical testing requirements (based on procedure invasiveness) and standard guidelines for evaluating abnormal test results.
- Risk-based management: Physicians also established pre-operative patient management protocols based on patient comorbidities.
- Business huddle: During a brief morning meeting, staff examine and adjust the upcoming schedule to ensure optimal efficiency and utilization.
- Operational huddle: A multidisciplinary team meets every afternoon to verify medical clearance for upcoming cases and resolve any outstanding issues.
Outcomes: Strong Improvement in Performance Metrics
The SSEC at Memorial Regional implemented OR changes throughout 2013. By the end of one year, these changes had produced dramatic improvement in several key performance measures.

Outcomes: Robust Improvement in Financial Performance
The SSEC at Memorial Regional implemented OR changes throughout 2013. By the end of one year, these changes had produced dramatic improvement in several key performance measures.

How to Achieve Unbeatable Performance
The transformation process at Memorial Regional followed a pattern that can be replicated in any hospital OR. Hospitals across the country have used these interventions to create a strong surgery department that drives the overall success of the organization. Key principles include:
- Reach out to surgeons. No OR can succeed without providing excellent service to its surgeon staff. When embarking on an OR transformation, involve surgeons early to understand their needs and enlist allies.
- Put physicians in charge of the OR. In our experience, when surgeons and anesthesiologists are given control of the OR, they make fair and balanced decisions that strengthen the department and increase its value to the hospital.
- Guard precious time resources. OR time is expensive. The top priority of any OR transformation project should be to create a block time system that rewards surgeons who use OR time efficiently.
- Build quality into the front end. Most OR efficiency problems stem from poor communication and coordination during the days and weeks before surgery. Well designed pre-operative processes yield strong gains in quality, efficiency, costs and physician satisfaction.
- Leverage gains to grow the OR. Effective leaders translate OR improvements into volume growth. An OR that can provide surgeons with an efficient, high-quality work environment is poised to be an unbeatable competitor within its market.



