Nearly every hospital and healthcare system in the US is paying a significant stipend for their anesthesia services. Surgical Directions is now seeing these stipends often exceeding $100,000 per anesthesia provider. With most hospitals facing significant financial headwinds, the pressure to reduce these stipends is more urgent than ever.
There are numerous reasons behind the current anesthesia stipend crises:
- Shortages of anesthesiologists, CRNAs, and AAs
- With the aging US population, increasing numbers of procedures, both within the OR and procedural services, requiring anesthesia services
- Rapid rise of the ASC, siphoning off significant numbers of better paying patients, leaving the hospital with more complicated patients with poorer payer mix
- Anesthesia management companies with significant overhead and profit margins that are passed on to the hospital
- Problematic anesthesia billing and collection practices
- Poorly managed groups with inappropriate staffing models
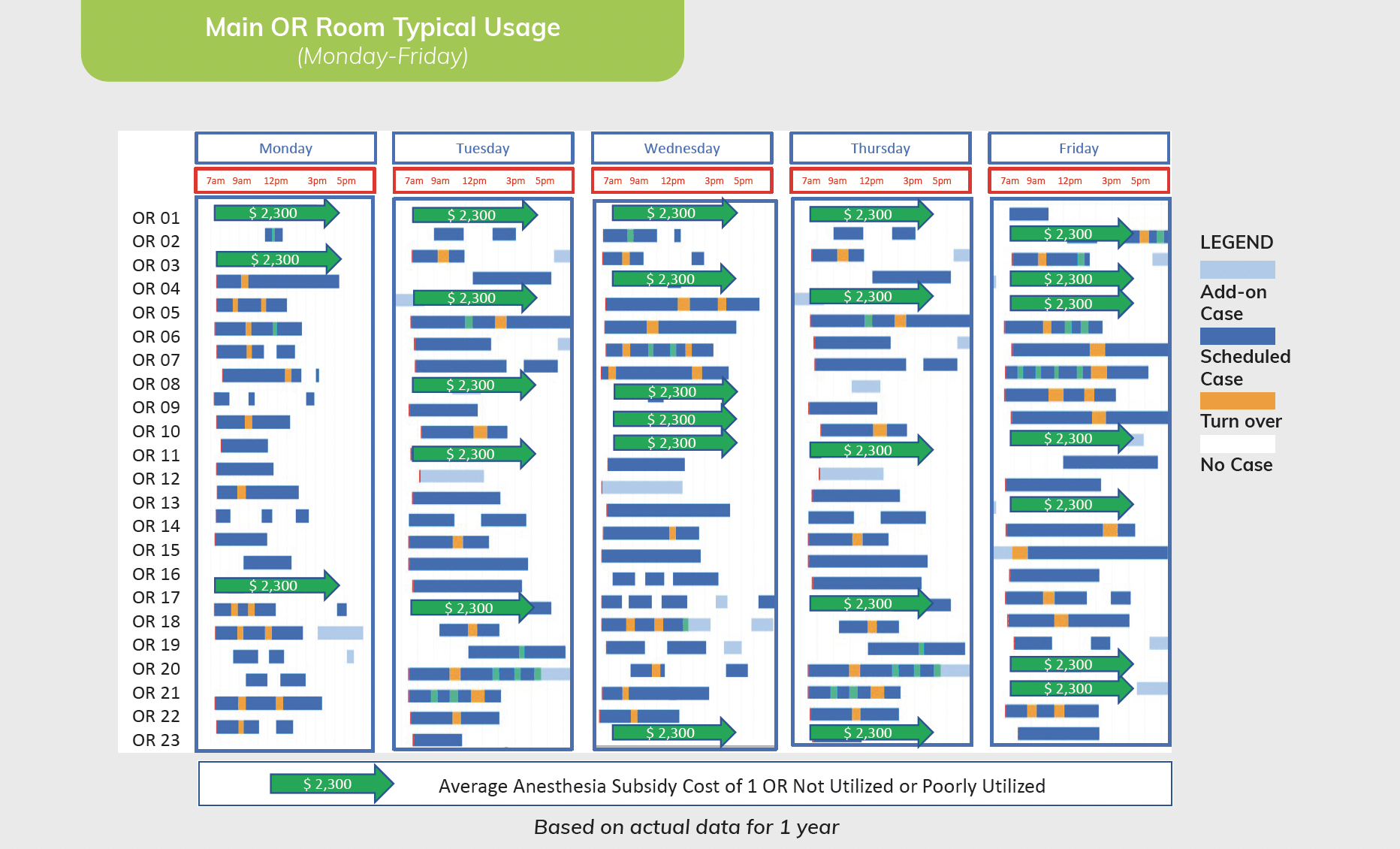 Additionally, an important component of these stipends is very often poor productivity (utilization) of procedural services, which include both the operating room as well as ‘non OR anesthesia’ cases (NORA). The NORA sites typically include the GI suite, cardiac cath. lab, interventional radiology, etc. Improving the productivity in these procedural areas will directly affect the anesthesia stipend in a very positive way for the hospital. Moreover, improving procedural services utilization will have a significant impact on the hospital overall bottom line. Let’s look at an example of how improving poor utilization of a hospital’s operating room can have a dramatic effect on the anesthesia stipend. The figure below is single week’s surgical usage within a 23-room operating room. By contractual arrangement with the hospital, the anesthesia department is required to staff these 23 operating rooms, whether filled or empty. Note the unused—but staffed—capacity. Unfortunately, for this hospital, this example is a regular weekly occurrence. A financial analysis revealed a $2300/room/day cost in fixed anesthesia overhead. In this example, applying these sunk costs over a 52-week year added up to $4 million in unused anesthesia capacity. Moreover, this example does not include losses from other fixed staff cost, such as nursing and support staff. From this real-life example, it should be obvious that addressing poor operating usage, can have a significant impact on your anesthesia stipend. However, most hospital administrations are either not aware of this issue or are leery of intervening into their surgeon’s use of the operating room. Managing a reallocation of surgeon access to your operating room to improve overall pro-ductivity/utilization is often viewed as a daunting and risky task, and traditionally avoided. Nevertheless, many hospitals are now faced with the alternative of either ad-dressing poor procedural services usage or continuing to descend into worsening financial condition. With the imperative that status quo is not sustainable, how does a hospital begin the process of improving utilization? It is a multi-step process:
Additionally, an important component of these stipends is very often poor productivity (utilization) of procedural services, which include both the operating room as well as ‘non OR anesthesia’ cases (NORA). The NORA sites typically include the GI suite, cardiac cath. lab, interventional radiology, etc. Improving the productivity in these procedural areas will directly affect the anesthesia stipend in a very positive way for the hospital. Moreover, improving procedural services utilization will have a significant impact on the hospital overall bottom line. Let’s look at an example of how improving poor utilization of a hospital’s operating room can have a dramatic effect on the anesthesia stipend. The figure below is single week’s surgical usage within a 23-room operating room. By contractual arrangement with the hospital, the anesthesia department is required to staff these 23 operating rooms, whether filled or empty. Note the unused—but staffed—capacity. Unfortunately, for this hospital, this example is a regular weekly occurrence. A financial analysis revealed a $2300/room/day cost in fixed anesthesia overhead. In this example, applying these sunk costs over a 52-week year added up to $4 million in unused anesthesia capacity. Moreover, this example does not include losses from other fixed staff cost, such as nursing and support staff. From this real-life example, it should be obvious that addressing poor operating usage, can have a significant impact on your anesthesia stipend. However, most hospital administrations are either not aware of this issue or are leery of intervening into their surgeon’s use of the operating room. Managing a reallocation of surgeon access to your operating room to improve overall pro-ductivity/utilization is often viewed as a daunting and risky task, and traditionally avoided. Nevertheless, many hospitals are now faced with the alternative of either ad-dressing poor procedural services usage or continuing to descend into worsening financial condition. With the imperative that status quo is not sustainable, how does a hospital begin the process of improving utilization? It is a multi-step process:
- It requires commitment and leadership from senior administration. This effort will need continuous guidance and administration sponsorship.
- Developing baseline procedural services productivity should be the next step. Best practice productivity definition is ‘adjusted utilization’ (AU), which is the ‘wheels in, to wheels out time’ + turnover time / allocated block time. This AU baseline should include all surgical volume including the elective schedule as well as the more urgent add-ons.
- Once overall and site/room- specific AU is calculated, establishing productivity goals comes next. For the typical hospital OR room, achieving 75% adjusted utilization, in all OR rooms, on all days of the week. In Surgical Directions’ experience most hospital operating rooms have AU of less than 75%, with most in the range of 50-65%.
- Next comes the hardest challenge, i.e., reaching consensus with surgeons, anesthesia, nursing, and senior administration on reallocation of surgeon access to reach the goal of 75% adjusted utilization. A multi-disciplinary task group is required to assess need, direction, and implementation steps (see SD blog on the SSEC)
- Once the new surgeon access system is in place, ongoing measurement of operating room productivity, efficiency and quality of care is required. This will require diligence and accountability.
The good news of this effort will be the improved productivity of your fixed-cost staff, likely significantly reducing your anesthesia stipend. In conclusion, there can be many reasons behind your rising anesthesia stipend. However, addressing poor utilization of expensive procedural services can have a major impact on anesthesia stipend, as well as other fixed-cost staff expense.



