Executive Summary
Cultural friction in the operating room creates high clinician and staff turnover, surgical case volume outmigration and patient care risk. So, no wonder it is one of the greatest complaints I hear about across the 500 or so U.S. hospitals that Surgical Directions and I have worked with.
Improving culture is necessary to deliver great surgical care…but you must play the ‘long game’. It takes a multi-faceted approach over months to truly get surgeons, anesthesiologists, nurses, administration, and staff effectively communicating, collaborating and building a strong culture.
It is worth the investment. We have implemented cultural transformation efforts at hundreds of hospitals across the country and have seen improvements not only in retention and satisfaction, but also in financial performance.
 On average, hospitals that have enacted these tactics have seen their primetime OR utilization increase by over 20% within six to 12 months following implementation.
On average, hospitals that have enacted these tactics have seen their primetime OR utilization increase by over 20% within six to 12 months following implementation.
Here are four tactics that can help to transform the culture of your surgical services departments.
Four Tactics to Transform Culture in Surgical Services
1. Establish a Collaborative Physician-run Governance Committee
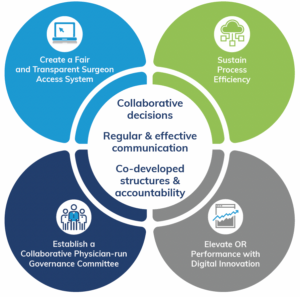
The culture of a procedural care department is defined by the behaviors of its constituents – surgeons, anesthesiology, nursing, staff and administration. When these groups are empowered to make collaborative decisions, communicate regularly and well and co-establish mechanisms to define success and hold each other accountable to it a better culture is created.
To start, create structures that encourage regular and constructive communications across the constituents. We recommend an operationally focused, administratively sponsored Surgical Services Executive Committee that is co-chaired by a surgeon and an anesthesiologist. Key players, like the OR Director and service line surgeons and leads, should be voting members. Through this committee, decisions on success metrics, surgeon access standards, OR operational management should be escalated, discussed, reviewed, voted on and socialized.
It is critical that a senior administrator sponsors and attends each meeting and empowers the physician co-leads to set the meeting agenda, lead the meeting, and lead the attendees to vote on key decisions. This will encourage attendance at each of the meetings and keep engagement high. It also helps to create a culture of accountability. Senior leadership can hold people accountable to decisions and use surgeon scorecards to measure and manage the committee process.
This governance structure can also scale across a health system, where each hospital-level governance committee rolls into a system-level surgical services executive committee. One way to do this is have the co-chairs of each hospital-level committee serve at the system-level to ensure bi-directional communication and accountability. The governance structures can also work for the non-operating room locations, like endo, I/R and labor & delivery.
2. Create a Fair and Transparent Surgeon Access System
Next, form a surgeon access subcommittee that reports into the Surgical Services Executive Committee.
This committee can help to establish and hold surgeons accountable to block policies and utilization targets. This group will also analyze surgeon scheduling and utilization patterns and identify their impact on block utilization. Many committees set a threshold of 75%-80% that a surgeon must use his or her block to keep that block during the next evaluation period. A lot of improving surgeon access is helping to build predictability so a hospital can deliver on surgeon expectations and improve the surgeon and nursing experience. Once you build in predictability, that is when you can get efficient and ultimately improve your bottom line and add room for growth.
3. Sustain Process Efficiency
We like to say “it’s better to get your house in order before you ask someone to change theirs.” The same applies to surgery. It’s hard to ask a surgeon to change when or how s/he does a procedure if the surgical department has slow turn-around times, surgical trays are missing instruments, or a patient is not appropriately prepped.
We saw hospital primetime utilization go up by nearly 20%, on average, through shorter turn-around times, improved patient preparation and better designed surgeon access schedules. This means great patient access, better utilization of resources and reduced overtime and waste. It also improves staff retention and stability of ORs.
To mobilize this type of change, we establish multi-disciplinary performance improvement teams that focus on areas like central sterile processing, materials management, OR throughput, and pre-anesthesia testing. We also recommend setting up a Collaborative Daily Review.
4. Elevate OR Performance with Digital Innovation
Most hospitals only use a fraction of the capabilities in their current information systems. Fully commit to a digital strategy that leverages technology in ways that contribute to OR efficiency, save costs, and boost retention.
Actionable analytical tools, like Merlin™, create powerful insights in areas such as workforce strategies, financial and operational decision-making, and patient experience improvements. For example, data-driven block scheduling helps create a more “vertical” schedule based on optimal utilization during primetime hours. This helps control nursing costs by reducing the OR’s dependence on travel nurses. It also helps ORs respond to the anesthesia provider shortage by allowing current anesthesia staff to cover rooms more efficiently, which can reduce the need for a financial stipend.
 One of our health system clients generated a 25% surgical volume jump upon leveraging Merlin™ to redesign the block schedule, re-allocate cases across the main OR and same day surgery centers, and improve surgeon access.
One of our health system clients generated a 25% surgical volume jump upon leveraging Merlin™ to redesign the block schedule, re-allocate cases across the main OR and same day surgery centers, and improve surgeon access.



