As we venture deeper into 2024, five topics have dominated the hospital executive’s mindshare. From financial recovery and workforce shortages to technological advancements and an emphasis on health equity, the current state of healthcare demands a fresh perspective and innovative strategies.
Through conversations with clients across the nation, Surgical Directions has created an overview of these critical focus areas:
Financial Burdens and Resilience: A Perfect Storm
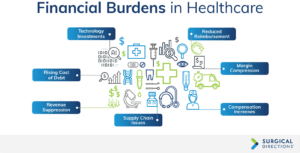
In the evolving landscape of healthcare, financial challenges remain the most pressing concern for hospitals and health systems. Margin compression—driven by decreased reimbursements and increased cost structures—has created a financial squeeze forcing health systems to make difficult decisions. While never wavering on the primary goal of providing the highest quality care for their patients, hospital leaders face financial pressures that require trade-offs, such as closing procedural care rooms or limiting purchases of new technologies.
Healthcare organizations, like most others, operate on a straightforward financial equation: Profit equals revenue minus costs. Most health systems are not-for-profit, meaning they do not need large margins, but they still need to cover their costs. Revenue, driven by patient volume and reimbursements, lags. Recent CMS announcements of slight reimbursement increases are still insufficient to offset rising care costs. As the top line decreases, the bottom line rises, and an already thin margin becomes more suppressed.
The cost structure of hospitals is climbing, significantly impacted by workforce shortages. Additionally, supply chain issues continue to inflate prices for essential materials and equipment. This financial strain forces hospitals to rethink care delivery and investment strategies. Some hospitals face bankruptcy, while others grapple with the rising cost of debt due to increasing interest rates. Decisions on whether to invest in innovation or prioritize current staff retention become more complex under thin margins.
Despite these challenges, there are signs of resilience. In 2023, healthcare sector margins improved from -0.5% in January to 2.3% by year’s end (Kaufman Hall), thanks to efficiencies and workforce solutions. The ability to adapt amidst financial constraints is crucial to maintaining high-quality patient care delivery.
Workforce Shortages: A Growing Crisis
Since COVID-19, workforce shortages have emerged as a critical issue in healthcare, affecting physicians, nurses, and technical staff. This shortage hampers the ability to deliver care at pre-pandemic levels. The challenge lies not only in attracting and retaining a workforce but also in fostering employee well-being.
Workforce shortages for physicians and nurses are not a new challenge. However, the pandemic exacerbated the problem, leading to significant departures from the workforce. Many part-time or alternative-schedule workers also exited the field, creating a serious supply issue. Regulatory changes affecting reimbursement structures have further burdened this situation, leading to a compensation mismatch between limited supply and growing demand. For instance, anesthesiologists and certified registered nurse anesthetists have seen a nearly 30% increase in compensation over the last few years, yet there remains a talent shortage of both professions, and hospitals are paying more to get less. This further strains their already thin margins.
Turnover has compounded the workforce issue. Some health systems have experienced up to 80% staff turnover since COVID-19. Extensive training programs such as Periop 101 have emerged to adequately and quickly prepare new staff. This turnover necessitates doubling up resources and investments to ensure quality remains high, despite a reduced workforce.
Mental health and well-being have become crucial areas. High-acuity patient care can be draining; creating safe working environments for staff to process their experiences is vital to prevent burnout. Hospitals and provider groups are increasingly focused on wellness platforms and initiatives to promote mental health among their staff.
Novel approaches, such as setting up “Getting Rid of Stupid Stuff” (GROSS) committees, aim to streamline processes by eliminating unnecessary tasks. This subtractive approach helps alleviate burnout and improve productivity by focusing on necessary activities and removing redundant ones. Daniel Pink, author of Drive, advocates for a “don’t do” list to enhance productivity by avoiding non-essential tasks.
Physician and nursing shortages are projected to worsen, with the Association of American Medical Colleges forecasting a deficit of up to 124,000 physicians by 2033, and the International Council of Nurses projecting a need for an additional 13 million nurses by 2030. While some strides have been made in reducing reliance on contract labor, the staffing landscape remains precarious. Addressing clinician burnout, enhancing employee wellness, and leveraging process solutions are key to retaining talent.
Cybersecurity: A Lurking Danger
The rise of sophisticated cyberattacks and their resounding effects have created immense worry around data protection. In 2023, ransomware attacks nearly doubled, impacting 141 hospitals and causing severe revenue disruptions. The American Hospital Association (AHA) described the Change Healthcare attack as the most significant cyber breach against a U.S. healthcare organization, prompting leaders to increase cybersecurity budgets and infrastructures. Incidents such as the CrowdStrike IT outage, which impacted multiple industries, underline the importance of robust cybersecurity measures across all sectors.
These notable events have exposed vulnerabilities within our sector, highlighting the need for robust cybersecurity measures. Hospitals are investing in solutions such as cybersecurity insurance, rigorous data protection protocols, and careful management of data sharing. The growing sophistication of cyber threats, including ransomware and phishing, has made this increasingly challenging. The need for cybersecurity experts has introduced new financial burdens for hospitals, contributing to industry consolidation. Smaller hospitals may struggle to afford the necessary protection, prompting mergers to share resources and expertise.
Understanding system interdependencies and educating patients, consumers, and employees about cybersecurity risks are essential. Continuous education helps everyone play a role in protecting sensitive information and maintaining trust in our healthcare systems.
Advancements in Technology: AI and Beyond
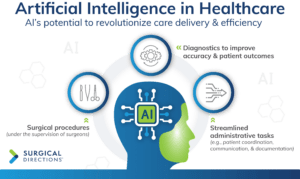
Rapid technology advancements—artificial intelligence (AI) in particular—is transforming healthcare. AI’s potential to revolutionize care delivery and efficiency cannot be ignored. It is crucial for hospitals and health systems to adapt to these changes by revising processes and behaviors accordingly.
AI’s integration into healthcare is reshaping how hospitals provide care, making it more accessible, efficient, and affordable. One significant advancement is the potential for AI to assist in surgical procedures—akin to unmanned surgeries—where robots perform operations under the supervision of surgeons. This technology builds on the longstanding use of robotics in surgery, enhancing precision and adaptability through data insights from numerous procedures.
AI’s impact extends beyond the operating room. It plays a crucial role across the care continuum, from symptom onset to post-operative care. AI can streamline administrative tasks, such as patient coordination and communication, traditionally managed by multiple staff members. AI also has a powerful future in diagnostics to improve accuracy. While human oversight remains essential, AI advancements promise significant improvements for patient outcomes.
Additionally, AI can reduce workforce burnout by decreasing administrative burdens. Automation in note-taking and updating electronic medical records saves valuable time for clinicians, reducing the so-called “pajama time” spent working after-hours. This savings enhances clinicians’ work-life balance, contributing to their overall well-being and ability to provide high-quality care during working hours.
Health Equity: A Core Imperative
 Health equity remains a significant challenge in the U.S. healthcare system, as underserved and lower-income communities often receive inferior care compared to higher-income areas. Other indicators of care inequity include gender and race. Addressing disparities is crucial for ensuring that all individuals have access to similar levels and quality of care.
Health equity remains a significant challenge in the U.S. healthcare system, as underserved and lower-income communities often receive inferior care compared to higher-income areas. Other indicators of care inequity include gender and race. Addressing disparities is crucial for ensuring that all individuals have access to similar levels and quality of care.
Healthcare providers play a pivotal role in advancing health equity. Hospitals, often major employers in their communities, have a unique position to drive change both as healthcare providers and community leaders. Collaborating with local organizations, schools, and other community services can help address broader social determinants of health, such as housing, food security, and safety, which contribute to overall well-being.
Staff education is also key in tackling health equity. Studies show that unconscious biases, such as discounting the pain levels of African American mothers, negatively affect outcomes. Raising awareness among healthcare professionals about these biases helps enhance listening, communication, and overall interactions with patients to ensure more equitable treatment plans.
Despite the complexity of the issue, incremental steps can make a significant impact. Initiatives like One World Surgery, which provides free surgical care to those in need, demonstrate how targeted actions can enhance access to healthcare for underserved populations. By offering their expertise in scheduling and efficiency, organizations can extend their impact, helping more patients receive the care they need.
Conclusion: A Path Forward
Considering these current trends, a path forward for hospitals involves addressing several key areas. As hospitals face financial burdens and margin compression, focusing first on areas most within their control, such as waste reduction, creates the best opportunity. For instance, surgical trays often contain items that go unused yet are sterilized and recirculated, leading to unnecessary expenses. By identifying and eliminating waste, such as reworking the surgeon preference card, hospitals can significantly improve efficiency. Implementing a “don’t do” list can also help eliminate redundancy. Additionally, process re-engineering—though time-consuming for a short period of time—can reduce waste without incurring extra costs. Utilizing existing technologies more effectively is another way to cut costs and enhance operational efficiency.
The ongoing talent shortage and employee burnout challenges require a focus on strong leadership and supportive work environments. Retaining current employees is easier and more cost-effective than recruiting new ones. Investments in employee well-being and fostering a healthy workplace culture are essential. Emphasizing behaviors that support these goals and holding individuals accountable to these standards can enhance job satisfaction and reduce turnover, leading to a more stable and motivated workforce.
Cybersecurity in healthcare is increasingly complex, with threats emerging from various sources. Education and training can mitigate some of the risk. Implementing robust safety structures within technological systems also protects against cyber threats. Collaboration, best-practice sharing across industries, and fostering a culture of cyber awareness can help organizations stay ahead of potential threats to ensure data remains secure.
As hospitals work hard to protect information, they balance rapid technology advancements, especially AI. Safe AI adoption offers significant opportunities for healthcare, from operational efficiencies to staffing support. Start with small, manageable projects and gradually scale up, prioritizing areas with the most significant challenges to ensure technology investments have the greatest impact.
Finally, our society faces systemic health equity issues, and hospitals are uniquely positioned to lead these efforts, connecting underserved populations with essential services. As major employers, healthcare organizations can work with community members to address disparities and bias. Partnering with local communities and tailoring care to specific patient populations can create more equitable healthcare environments. Focus on attainable initiatives and build upon them to make meaningful, long-lasting progress in our communities.